Health Care for 1% of the Cost
There is a general consensus that U.S. healthcare needs major reform. Can reverse innovation — innovations originating from poor countries — provide one important answer? Most definitely.
"Can reverse innovation — innovations originating from poor countries — provide one important answer? Most definitely."
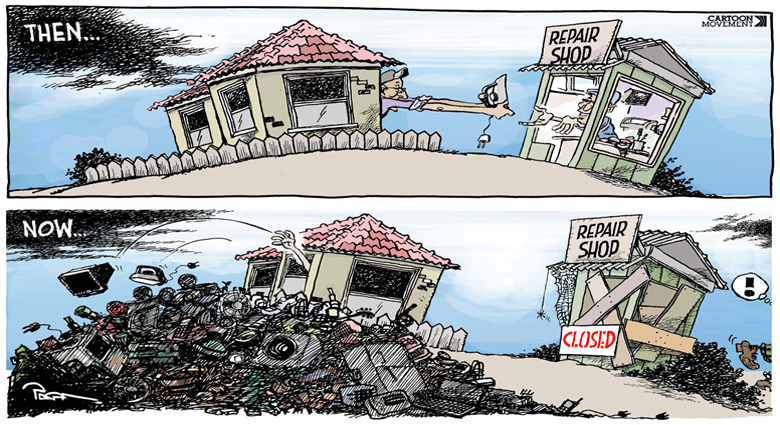
In the U.S., the approach is to spend more money on major technological advances and come up with innovative products and solutions. In poor countries, the innovation paradigm is just the opposite: spend less and innovate new business models. Poor countries face severe resource constraints. They just cannot afford to spend a lot. Constraints need not be limiting, they can actually be liberating.
The ultra low-cost, high-quality prostheses innovation of Dr. Therdchai Jivacate and the Prostheses Foundation of Thailand is an inspiring example of this. Over the years, they have developed and delivered over 25,000 affordable and appropriate artificial legs to amputees in remote areas of Thailand and surrounding countries. In the U.S., an artificial leg costs about $10,000 and the delivery time is 7-10 days. The Prostheses Foundation of Thailand is able to do it for less than $100, about 1% of the U.S. cost, and their delivery time is 1-3 days.
Though Dr. Jivacate spent four years as a resident of physical medicine and rehabilitation in Northwestern University, he understood that conventional artificial legs were unaffordable and inappropriate for the majority of Thai amputees. There are several reasons. First, customers in rural Thailand simply cannot afford to pay a high price. For the poor making $2 a day, a $10,000 product would require 5,000 days of income. (With 200 working days a year, that amounts to an incredible 50 years). Second, the context and functional requirements for amputees in Thailand are vastly different from those in the U.S. Thai people do many of their daily activities with bare feet, sitting squat on the floor or cross-legged, and many work in wet paddy fields. Furthermore, while many roads in the U.S. are paved, Thai people walk on uneven roads. Finally, the expensive artificial legs are only available in Bangkok, thus making it virtually inaccessible to the rest of the population.
Dr. Jivacate defined the most essential customer problem: to be able to walk without pain. He set out to develop a solution. His mission was not just to reduce costs — but to shift the price-performance paradigm. Actually, the artificial leg has to be higher-quality than in the U.S. to meet the more demanding functional requirements in Thailand, yet it has to be ultra low-cost. How did he achieve such an impossible goal?
There are two major cost drivers in an artificial leg — raw material cost and the cost of technicians.
Dr. Jivacate realized that he could not achieve his goal with expensive materials such as titanium, which is used in rich countries. One of his technological breakthroughs was to make artificial legs from recycled plastic yogurt bottles. These artificial limbs were extremely cheap. Raw material cost was close to zero since he used waste. More importantly, the limbs were lightweight, durable and comfortable. Dr. Jivacate converted waste into wealth.
He also knew that professionally-skilled technicians were in short supply and too expensive to hire. Dr. Jivacate therefore instituted training programs for those amputees who showed a special interest in the fitting process. He hired amputees as technicians to do the fitting and help with rehabilitation and training with new patients. This approach had several benefits. First, it dramatically reduced costs. Second, the amputee-technicians approached their work with passion since they personally benefited from the product. Third, it stimulated the demand for the product since these technicians could credibly convince patients that the product works. Fourth, it improved quality since Dr. Jivacate's technicians understood, based on personal experience, how to fit the prosthetic leg without pain and discomfort. Dr. Jivacate's technicians were thus most customer-centric. Fifth, they understood customer feedback, which led to continuous process improvements. Sixth, it created an instant empathy and a high degree of trust between the amputee-technicians and the patients. Finally and most importantly, it created much-needed job opportunities for the poor.
He also re-invented the delivery model. Patients in remote areas of Thailand could not afford to travel to clinics in an urban setting. So, Dr. Jivacate innovated highly-efficient mobile clinics and 27 satellite workshops in local areas. Between 1992 and 2011, the mobile units have made more than 115 trips serving over 16,000 amputees. It has recently broken the Guinness Book of World Records by serving 864 amputees in 13 days.
Finally, Dr. Jivacate tailored the devices to meet unique local needs — for instance, he custom-built artificial legs specifically for farmers who worked in wet fields.
Originally targeting the poor, continuous innovations have drastically improved the quality of the artificial legs over time (ISO certificates pending). The limbs are now also used by more affluent amputees in Thailand and in other neighboring countries such as Indonesia, Malaysia, Laos, and Burma.
In addition to treating humans, Dr. Jivacate fabricated a prosthetic leg for Baby Mosha, a 7 month-old elephant, who was injured in a landmine in 2009 — a remarkable medical achievement captured in the award winning documentary film The Eyes of Thailand.
If we can make an artificial leg for an elephant for less than $100, why does a less complicated procedure for humans have to cost $10,000?
This story is not an isolated example. In India, for example, Aravind Eye Care does cataract surgery for $30, compared with as much as $1,000 in the rich world. Bangalore-based Narayana Hrudayalaya Hospital performs high-quality open-heart surgery for just $2,000, compared to upwards of $20,000 in the U.S. Partners In Health (PIH) provides high-quality, ultra low-cost home-based services to the sickest and most marginalized HIV/AIDS patients in the U.S. — based on innovations PIH originally developed in Rwanda. Clearly, doctors in India and Rwanda do not know anything more about the science of eye care or cardiac surgery or treating HIV/AIDS patients. But they do know how to deliver quality care at lower cost. By comparison, there is something highly inefficient about the health care delivery in the U.S. — and much to learn from poor countries.
This blog post is written with Pepijn Veling, Utrecht University, Netherlands.





.png)


What Did You Think?